Mending a broken ‘system’ to learn lessons following inquests
Despite death being a universal experience, the function of the coroner service and the process of an inquest are relatively unknown until one personally experiences loss under tragic circumstances - i.e. an unexpected, unnatural, or unexplained death.
The current ‘system’
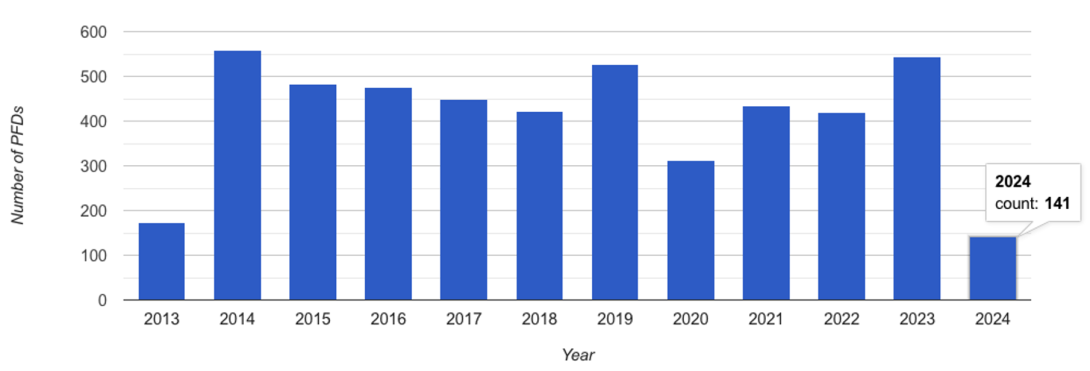
During or following an inquest, coroners in England and Wales send reports to individuals or organisations that they believe have the power to take action to reduce the risk of further deaths. These reports, called Prevention of Future Deaths reports or PFDs, and their responses have been made publicly available on the Judiciary website since July 20131. This information sits statically online with no oversight or ability to analyse trends and learnings from the reports.
There is no inspection of the quality or content of reports, and no follow-up to ensure responses are received and that actions are taken to prevent future deaths. These issues and the inadequacies of the ‘system’ have been well-documented for decades, with very little (if any) progress or reform. This lack of a ‘system’ to harness lessons following a tragic death comes as a shock to the bereaved, and the thousands of people with whom I’ve used my platform2 to share my insights on the broken system.
Mending the ‘system’
The UK is hailed as having some of the best healthcare databases in the world. So when I migrated from Australia in 2017, I was delighted to receive the opportunity to explore these datasets during my Doctor of Philosophy (DPhil/PhD) research that investigated the use and harms of strong pain medicines called opioids3. I found that opioids were being prescribed and used at increasing levels, which were contributing to rising death rates.
When investigating deaths in healthcare, data from the Office of National Statistics (ONS) or electronic health records from hospitals and general practice are used. However, these databases do not provide insight into the evidence presented during inquests or the concerns raised by coroners regarding the risks of further deaths. During my PhD, I discovered that there was no database or system to collect information from inquests or coroners’ reports, which could be routinely used for research and to inform policy as there was at home in Australia.
The final chapter of my PhD aimed to fill this gap, to capture information from coroners’ reports and synthesise data that would help reduce the rising deaths from opioids4. This chapter was the catalyst that led to the creation and publication of the Preventable Deaths Tracker platform.
Preventable Deaths Tracker
The Preventable Deaths Tracker is the first and only accessible database of all published coroners’ PFD reports in England and Wales. It automatically collects information from the Judiciary website every Sunday, which is converted into a usable and searchable database that contains over 10 years of data. It provides real-time analytics and statistics on coroners’ reports that were previously unknown and very difficult to obtain.
The Tracker also enables research and thematic analyses into particular areas of concern. Thus far, we have investigated self-inflicted deaths/suicide5, cardiovascular diseases6, medicines7, falls8 and sepsis9, with many studies ongoing. However, all research, work, and time spent building the Preventable Deaths Tracker has been self-funded and voluntary.
While 36,300 inquests opened in 2022, coroners’ PFD reports represented only 1.2% of all inquests. Therefore, these reports provide a very selected insight into the unexpected, unnatural, and tragic deaths investigated by coroners in England and Wales.
An ideal system
In Australia and New Zealand, all recommendations made by coroners during and following an inquest have been captured in the National Coronial Information System (NCIS)10 since 2000. The NCIS is routinely used for research, surveillance, and monitoring of deaths, which has significantly impacted policy, including reforming manufacturing policies, regulatory changes, awareness campaigns, and suicide prevention initiatives.
In comparison, the English and Welsh ‘system’ is at least 24 years behind the Antipodeans, and instead relies on the goodwill of volunteers, charities, and the bereaved to take action to prevent future deaths. While the current ‘system’ fails the dead and the living, the Preventable Deaths Tracker is evidence that more can, and must, be done to learn lessons following inquests.
[1] https://www.judiciary.uk/prevention-of-future-death-reports/
[2] https://preventabledeathstracker.net/
[3] https://www.cebm.ox.ac.uk/research/projects/an-evidence-based-approach-to-assess-the-use-of-opioids
[4] https://doi.org/10.1093/pubmed/fdad147
[5] https://doi.org/10.1016/j.puhip.2024.100491
[6] https://doi.org/10.3399/BJGPO.2021.0150
[7] https://doi.org/10.1007/s40264-023-01274-8
[8] https://doi.org/10.1093/ageing/afad191